When employees leave coverage, Vimly makes the COBRA experience clear, compliant, and easier to manage for both employers and former employees. Our full-service solution handles every required step so you can stay aligned with federal regulations and avoid costly mistakes.
We monitor regulatory changes, generate the required notices, and manage coverage updates, communication, payments, and carrier reporting. Your team can stay as involved or as hands-off as they prefer — we take care of the details.
Let Vimly help you manage the complexities COBRA administration so your HR professionals can focus on what matters most.
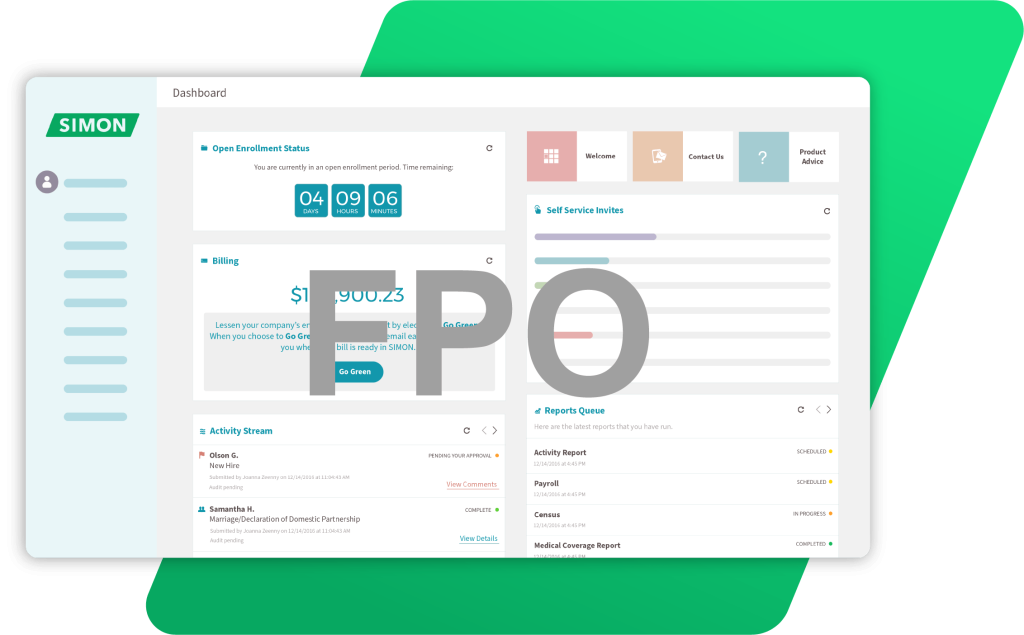
See how Vimly’s COBRA services, supported by the capabilities of the SIMON platform, can simplify administration and create a smoother coverage experience for former employees.